In the healthcare sector, where information loss can erode patient trust and lead to massive fines, HIPAA compliance is essential to protect sensitive information during communications. HIPAA-compliant call centers ensure that protected health information (PHI) remains secure, whether in inbound queries or outbound reminders. According to recent statistics, 444 reported cyber incidents affected healthcare in 2024, including 238 ransomware threats.
And after you get attacked, if a judge determines you were negligent in protecting info, you could be in trouble. For example, in 2015, Anthem Inc. faced a $16 million violation fine after hackers exposed nearly 79 million records due to inadequate safeguards.
This guide seeks to help your business avoid these issues by diving into HIPAA compliance requirements for call centers, essential features in HIPAA-compliant call center software, and operational best practices to maintain a secure contact center.
Key takeaways
- The law protects information: HIPAA compliance in call centers safeguards protected health information from unauthorized access, preventing unauthorized disclosure in healthcare call centers.
- Mandatory for those you work with: Any contact center handling PHI must meet privacy and security rules as a business associate.
- Fines are steep: Penalties get up to $71,162 per violation, with annual caps exceeding $2 million for repeated data breaches.
- Enhances operations and trust: HIPAA-compliant call centers improve efficiency with secure features like encryption, while fostering patient loyalty through transparent handling of health information.
- Ongoing training is key: Regular audits and agent certification in HIPAA compliance ensure call centers avoid common pitfalls and maintain robust safeguards against unauthorized disclosure when working with patients.
Understanding HIPAA compliance in call centers
What is HIPAA?
Short for the Health Insurance Portability and Accountability Act. It is a U.S. federal law enacted in 1996 and signed by President Bill Clinton. It protects information and promotes insurance portability. The law is primarily enforced by the Department of Health and Human Services. Its Title II establishes the Privacy Rule and Security Rule to safeguard health information from unauthorized access.
What is protected health information (PHI)?
PHI (Protected Health Information) refers to any health-related data that can identify an individual. It is governed by the law to prevent unauthorized disclosures or unauthorized disclosure and must be handled with strict safeguards. It includes things like:
- Patients’ names when combined with medical record numbers, a common example in patient data logs.
- Lab results or treatment plans discussed over calls; this is sensitive healthcare info.
- Phone call transcripts containing symptoms or diagnoses.
What HIPAA means for call center operations
The law profoundly influences contact center operations when speaking with patients by mandating secure protocols for handling patient data, requiring the use of encrypted communications:
- Scripts: These must incorporate the “minimum necessary” rule, disclosing only essential healthcare info, while agents follow verification steps to avoid unauthorized disclosure.
- Technology: Tech like secure VoIP and audit logs enable compliance, with business associates conducting regular risk assessments.
- Agent behavior: Noncompliance can halt operations, as seen in cases where data breaches led to OCR investigations, emphasizing the need to integrate these requirements seamlessly into daily workflows.
Who needs a HIPAA-compliant call center?
Lots! Healthcare organizations and any given contact center working with a patient must be compliant. This includes hospitals, clinics, and insurers. Some more include:
- Telehealth providers which offer patients virtual consultations, even if only for appointment scheduling involving key information.
- Third-party BPOs processing healthcare info of patients need BAAs (Business Associate Agreements) to formalize responsibilities.
- Dental offices with front desk schedulers discussing treatments, or pharmacies managing prescription calls, also fall under this, as they must ensure no data breaches occur.
Why trust matters in HIPAA-compliant call centers
Cost of noncompliance: fines, lawsuits, and reputation loss
Noncompliance, by a provider or by a healthcare call center, can lead to tiered fines, and a HIPAA complaint call from a patient can cost you: $100–$50,000 for unknowing violations (yes – you can receive a HIPAA complaint call even if you did not realize you broke a rule), escalating to $71,162 for willful neglect, with annual caps at $2 million. Advocate Health Care was the recipient of a (read: lots) HIPAA complaint call and was found to have lax safeguards; this led to their 2016 $5.55 million settlement after stolen laptops exposed 4 million patient records.
A HIPAA complaint call from one or more patients can damage your company’s goodwill. Plus, those aforementioned fines from affected patients raise costs for consumers, and reputation loss from data breaches can deter clients – creating a rather unpleasant spiral. You do not want a HIPAA complaint call about your healthcare call center.
How compliance improves satisfaction and loyalty
HIPAA compliance for call centers boosts patient satisfaction by ensuring secure, empathetic handling of healthcare info. Current trust in the medical field is plummeting in polling, and being HIPAA-compliant by sticking to these guidelines can help keep the trust you have. Instead of getting a HIPAA complaint call, you can get positive responses.
When you run a HIPAA-compliant call center and deal honestly with patients, transparent privacy practices build emotional connections, reducing anxiety over unauthorized disclosure and fostering long-term loyalty through reliable business associate partnerships.
HIPAA compliance requirements for call center software and operations
HIPAA compliance for call center software and operations demand comprehensive safeguards to protect data, including administrative policies, technical features, and physical controls to prevent unauthorized disclosure.
Patient communication rules
Patient communication rules are central to being HIPAA-compliant. Rules restrict PHI disclosures to treatment, payment, or operations, requiring explicit consents for other uses. You must document authorizations and limit healthcare info shared. Call center HIPAA violations can trigger unauthorized disclosure, hurting patients, so contact centers enforce “minimum necessary” standards across platforms.
Routine voice calls don’t need special consent from patients when not related to payment, but those which are unrelated to treatment/payment need written authorization. Texting requires opt-ins from patients (and they must be informed of any risks). This ensures data remains protected from unauthorized access.
Inbound & outbound calls
Both contact center types – those which deal with inbound and outbound calls from patients – must document patient HI handling, with agents verifying identities using multi-factor methods like DOB or account numbers. You can log these steps, which prevents unauthorized disclosure in discussions of healthcare info. Follow the law and call confidently without worrying if the call is going or coming.
Automated calls
Automated calls to patients don’t bypass the law; they require prior consents from patients. A HIPAA-compliant call center can use auto dialers when communicating with patients legally, but also cautiously, in order to avoid violations in your healthcare call center.
Call recordings
Call recordings stored by a contact center require patient consents, but do not need to be stored for a specific amount of time (state laws may vary); compliance documentation, however, must be stored with encryption for 6 years, per retention rules. This includes protecting access to call center software logs and tamper-proof storage to prevent unauthorized disclosure of recorded healthcare info.
SMS & MMS
SMS & MMS sent by a contact center to patients demand opt-in consents and limited PHI in messages, as appointment reminders can break the rules.
Administrative safeguards
Administrative safeguards involve developing policies, conducting risk assessments, and maintaining training logs to help protect patients. While some of these are part and parcel of good call center software, some will require training. BAAs are a necessity here, as is establishing incident response plans, which can help to ensure accountability for data protection.
Technical safeguards
Technical safeguards mandate features like firewalls and antivirus to secure PHI.
| Requirement | Control |
|---|---|
| Access Control | RBAC to limit PHI |
| Audit Controls | Logs for activity tracking |
| Integrity | Checksums for data verification |
| Transmission Security | Encryption for calls |
End-to-end encryption and secure call recording
End-to-end encryption used by a HIPAA-compliant call center ensures PHI remains secure during transmission with at least AES-256 standards. Secure call recording adds layers like watermarking to prevent tampering, essential for a healthcare call center.
Role-based access control and IAM
Role-based access control and IAM restrict PHI to authorized roles, enforcing least privilege principles. This minimizes internal unauthorized disclosure for handling patients healthcare info.
Data retention, backups, and breach protocols
Data retention requires 6-year storage of patients HI, with automated backups. These protocols mandate 60-day notifications, helping respond to unauthorized disclosure effectively.
Healthcare system integration
Healthcare system integration with EHR and CRM allows secure PHI transfer, ensuring encrypted APIs in contact centers.
Physical and remote access controls
Physical access controls can include locked servers, while remote access can include the use of safeguarded VPNs, and sometimes even biometrics and session timeouts.
Operational best practices for HIPAA call center compliance
Operational best practices when it comes to protecting patients involves a focus on proactive measures to protect data, including regular software updates. When talking to a business associate, emphasize continuous improvement to avoid unauthorized disclosure.
Train and certify call center agents regularly
A HIPAA-compliant call center should train and certify call center agents regularly (quarterly is standard) on PHI handling, breach reporting, and identity verification. Your contact center should hold a regular HIPAA rules call whenever there are big changes in regulations. Track certifications, ensuring that any given business associate complies.
Verify caller identity consistently
Verify caller identity consistently using methods like DOB, last four SSN digits, or appointment codes to safeguard PHI. This can help ensure you’re speaking with the right patients. Heed HIPAA and call with the intent to verify everyone you speak with.
Standardize secure omnichannel communication
Standardize secure omnichannel communication with patients and internally by using encrypted phone, webchat, and SMS in cloud call centers. You should log all channels and use safe call center software, protecting healthcare info from unauthorized disclosure.
Perform regular audits and internal monitoring
Perform regular audits and monitor call recordings with patients (and internal calls), agent activity, and access logs to detect any gaps. You can use contact center software to do this. Have your partners use dashboards to review data handling quarterly.
Best practices for building patient trust through compliance
Using transparent privacy policies and empathy in scripts
Using transparent privacy policies and empathy in scripts builds trust with patients. Include phrases like, “Your information is protected, here’s how.” Train your agents via to convey care, reducing patient anxiety over unauthorized disclosure.
Balancing personalization with data security
Balancing personalization with data security means using patient preferences without excess PHI collection.
- DO: Reference past appointments with patients without consent.
- DON’T: Share unverified details, risking unauthorized disclosure of patients’ info.
- DO: Explain any rights the patient may have when it comes to their data.
- DON’T: Speak on the speakerphone with patients, especially around individuals not cleared to be exposed to PHI.
How to evaluate healthcare call center software
Core compliance features to look for in call center solutions
These include encryption, audit logs, and third-party audits like SOC (Service Organization Control), which ensure robust protection of data.
Encryption, session management, and audit trails
Encryption secures data in transit, session management times out inactive users, and audit trails log all activity. SOC2 validates these for preventing unauthorized disclosure.
System integrations and automation support
Call center software integrations with EHRs and automation for consents streamline workflows. HITRUST certifies secure data flow for your contact center.
Compliance certifications
Compliance certifications like HITRUST and SOC2 help meet standards for PHI protection. These validate data security against unauthorized disclosure.
Red flags when evaluating HIPAA-compliant software
Red flags when evaluating HIPAA-compliant software:
- Missing encryption: Leaves patients’ info vulnerable to breaches.
- No audit logs: Hinders tracking of access.
- Lack of BAA support: Avoid software without these to protect data.
Scaling HIPAA compliance: from startups to enterprise needs
Scaling HIPAA compliance from startups to enterprise involves modular features like user permissions that expand. Startups focus on basic encryption, while enterprises add advanced audits to handle volume without increasing unauthorized disclosure risks. But all companies can engage in training and holding a regular HIPAA rules call.
Top HIPAA-compliant call center software options
Top HIPAA-compliant call center software options provide solutions for small teams and big ones when it comes to PHI management. Below is a comparison:
| Provider | HIPAA Compliance | Suitable For | Starting Price | G2 Rating |
|---|---|---|---|---|
| MightyCall | Yes | Small-medium healthcare | $20/user/mo | 4.5 |
| JustCall | Yes | Telehealth | $29/user/mo | 4.3 |
| NICE CXone | Yes | Enterprise | Prices vary | 4.4 |
| Five9 | Yes | Large call centers | $159/user/mo | 4.2 |
MightyCall
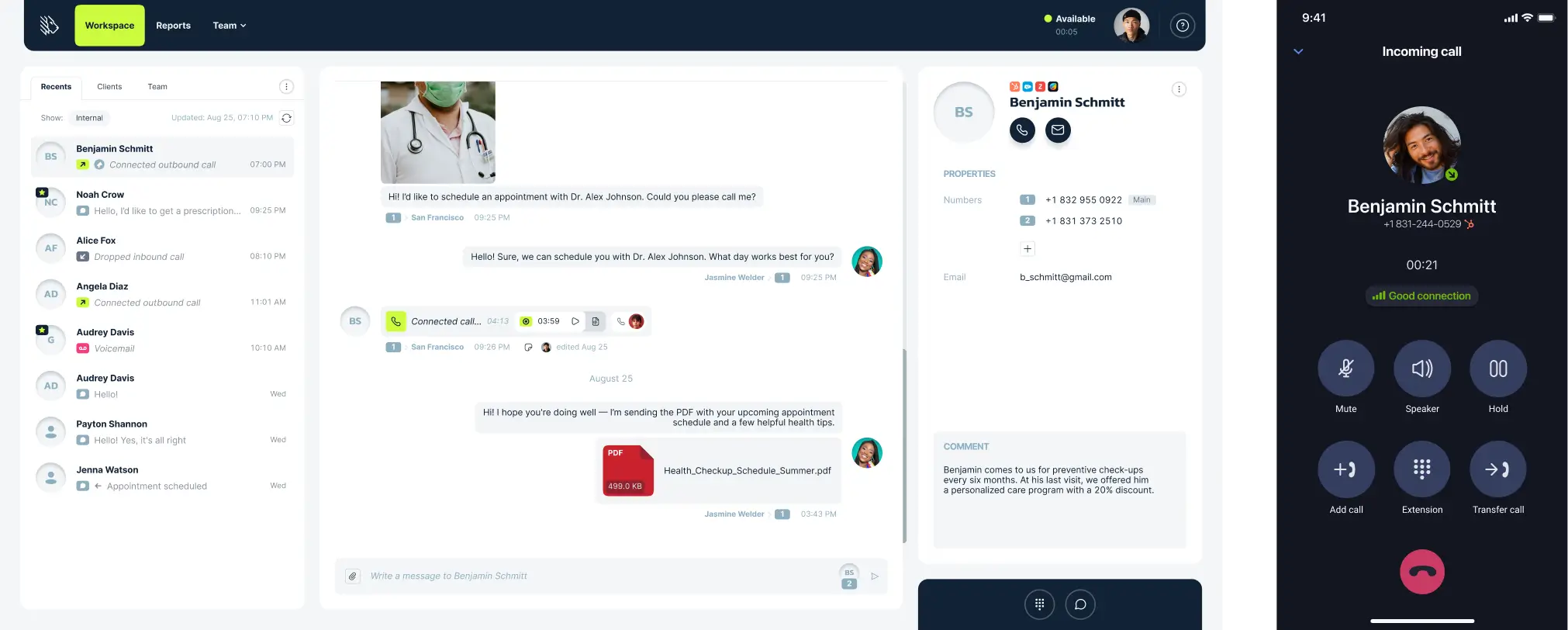
MightyCall offers HIPAA-compliant call center software with IVR, encryption, and mobile apps for secure data.
Compliance notes: BAA included, SOC2 certified. Suitable for a small or medium-sized healthcare call center.
G2 rating: 4.4/5
JustCall
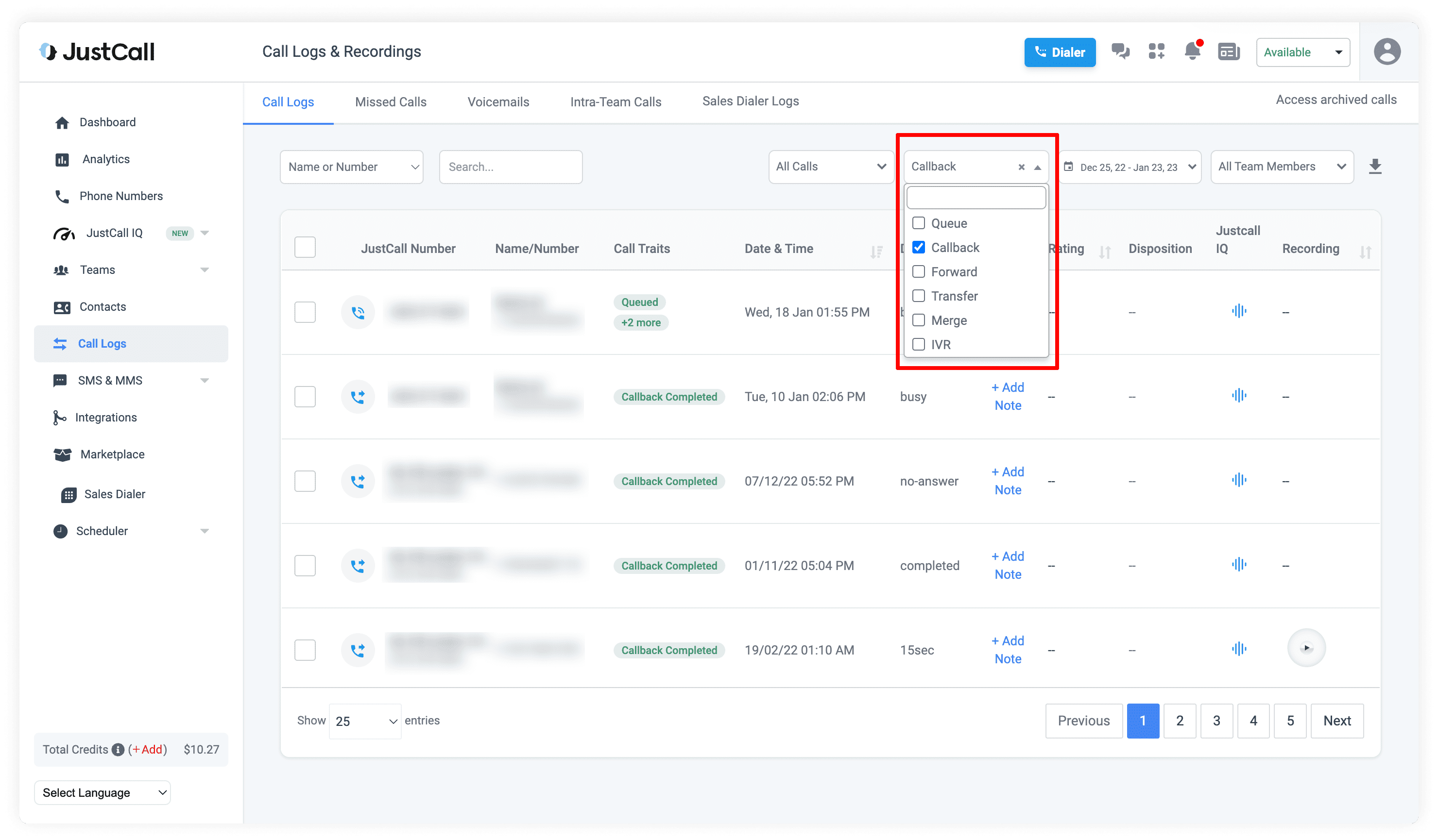
JustCall provides AI analytics and EHR integrations for healthcare info.
Compliance notes: BAA, end-to-end encryption.
G2 rating: 4.3/5
NICE CXone
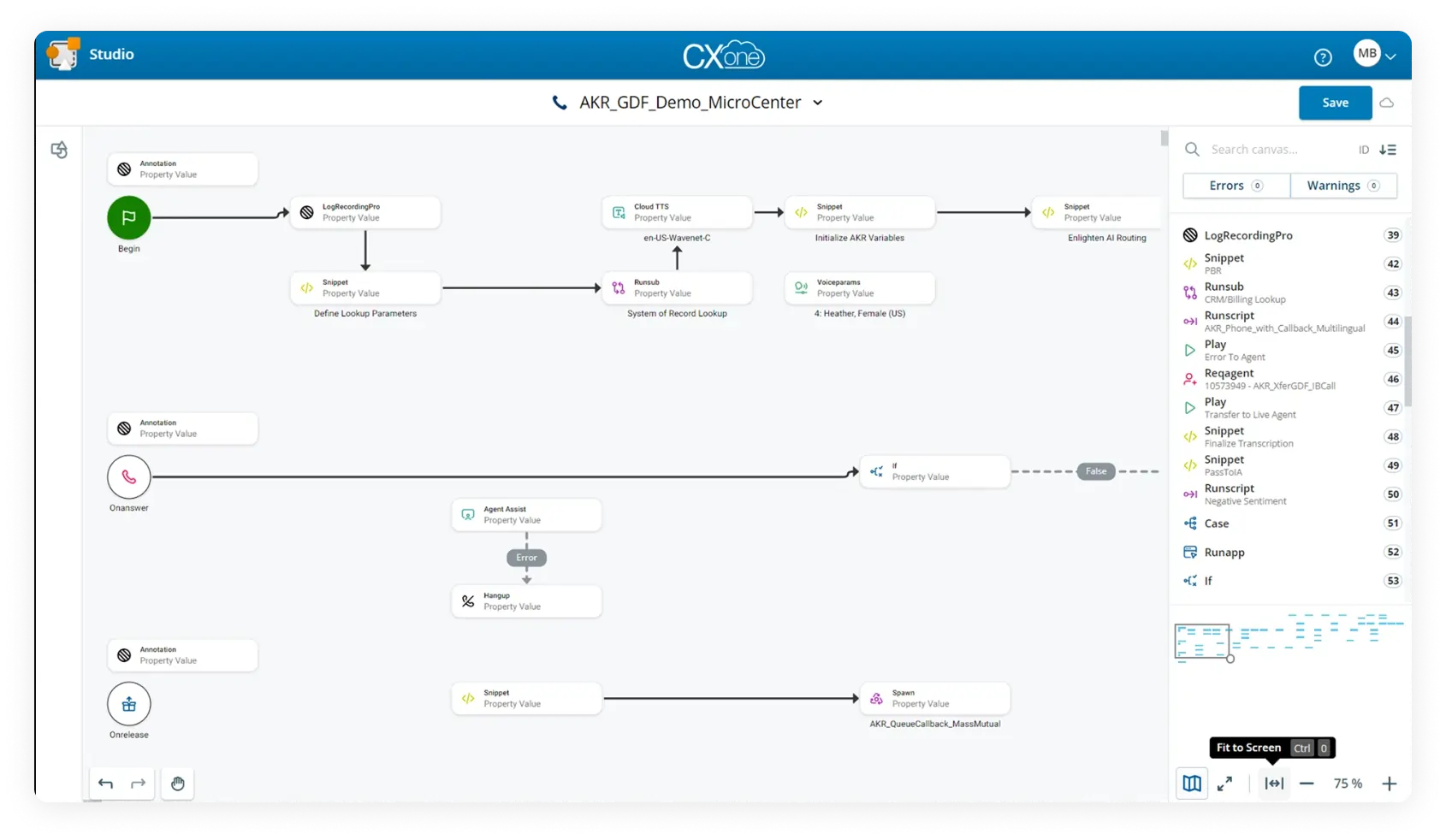
NICE CXone delivers, with omnichannel and dashboards for PHI.
Compliance notes: BAA, HITRUST.
G2 rating: 4.3/5
Five9
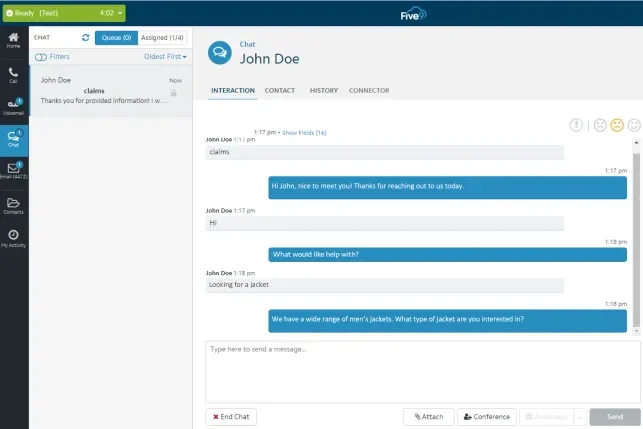
Five9 features intelligent dialing and integrations for patient data.
Compliance notes: BAA, SOC2.
G2 rating: 4.1/5
Checklist: Minimum compliance standards for call centers
Obviously you should seek to go above and beyond, but if you’re just starting out, these are the minimum standards you MUST meet. And we mean that: meeting these is a baseline, not optional:
- Sign BAAs with covered entities
- Encrypt all communications
- Train agents annually on PHI handling
- Implement access controls for data
- Conduct quarterly audits to prevent unauthorized disclosure
- Establish breach notification protocols within 60 days
- React quickly to any given HIPAA complaint call
- Use secure backups
- Verify caller identities consistently (as in every time someone speaks with the person)
Compliance roadmap: implementing HIPAA call center practices
Step-by-step implementation timeline
Phase 1: Assessment and planning (weeks 1-4)
This involves auditing current operations for PHI risks and selecting the right tools. You should identify any security vulnerabilities in your contact center.
Phase 2: Policy and software updates (weeks 5-8)
This includes drafting policies and ensuring you have encryption up and running.
Phase 3: Team training and go-live (weeks 9-12)
Here, you’ll certify agents and launch the system, testing for unauthorized disclosure in contact centers.
Phase 4: Ongoing monitoring
Ongoing monitoring which requires monthly audits and technical updates, ensuring long-term protection of data. If you get a HIPAA complaint call, rectify the issue immediately.
Common compliance pitfalls to avoid
| Pitfall | Result |
|---|---|
| Vendor lock-in without audit access | Leads to undetected unauthorized disclosure, violating the law |
| Untrained agents handling sensitive workflows | Increases unauthorized disclosures, risking fines |
| Lack of post-deployment audits | Allows ongoing vulnerabilities, exposing data |
Treating HIPAA as a strategic advantage
Lots of laws seem like useless, bureaucratic red tape. But this law can actually help you as a business owner, both for your own internal organizational purposes and in terms of client trust. It forces you to really be aware of who has access to what info, helping you to keep everything in-line. Plus, the trust it engenders, attracts more customers, provides for positive word of mouth, and fosters growth. Proactivity reduces unauthorized disclosure, enhancing brand trust and patient retention.